
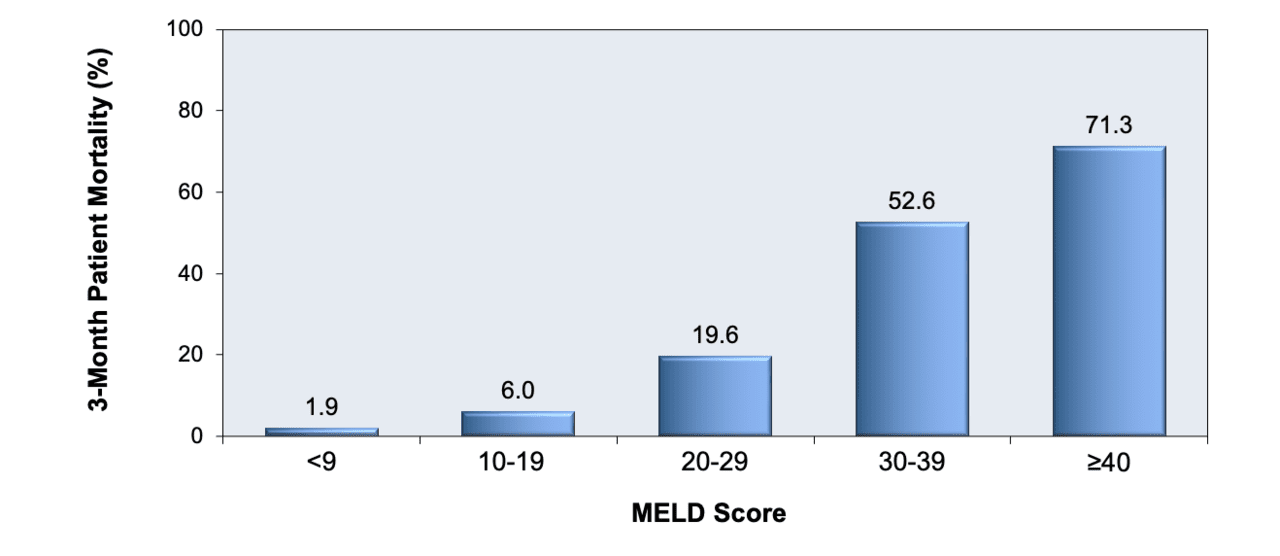
Specific therapies such as corticosteroids and pentoxyfilline need to be considered as they may reduce mortality in those patients who are at high risk of dying. The treatment of alcoholic hepatitis is largely symptomatic, with emphasis on alcohol abstinence and meticulous attention to nutritional status. In severe cases, alcoholic hepatitis is associated with a high mortality. A MELD score of greater than 11, or the presence of both ascites and an elevated bilirubin greater than 8 mg/dL should prompt consideration of specific therapeutic interventions to reduce mortality.Īlcoholic hepatitis is a manifestation of alcoholic liver injury characterized by necrotizing inflammatory hepatic lesions and acute hepatic decompensation. The MELD score performs as well as the DF in predicting mortality at 30 days. ConclusionsĪlcoholic hepatitis remains associated with a high mortality in hospitalized patients. The presence of ascites and bilirubin greater than 8 mg/dL were also highly predictive of mortality with a sensitivity of 71% and a specificity of 96%. However, the sensitivity and specificity in predicting 30-day mortality for a MELD score of greater than 11 was 86% and 81%, but for a DF greater than 32 was 86% and 48% respectively. The area under the curve of a receiver operating characteristic curve for the MELD score was 0.82 (confidence intervals 0.65–0.98), and for the DF was 0.86 (confidence intervals 0.70–1.00). We assessed the utility of the MELD score and compared it with the Discriminant Function (DF) as a predictor of mortality in 34 patients hospitalized with alcoholic hepatitis. Our aims were to assess the utility of the MELD score as a predictor of short-term mortality in persons with alcoholic hepatitis. The Mayo End-Stage Liver Disease (MELD) score is a marker of disease severity and mortality in persons with chronic alcoholic liver disease. Specific therapies should be considered for those at high risk of mortality. I use it to help patients understand their life expectancy, the need for listing or not listing, and for prioritizing patients on the waiting list.Īny other research in the pipeline that you’re particularly excited about?Įxpanding with other parameters, looking at benefits, and extending indications so we have a dynamic model.Alcoholic hepatitis is characterized by acute, or acute-on-chronic hepatic failure and associated with a high mortality. How do you use the UKELD Score in your own clinical practice? Can you give an example of a scenario in which you use it? To use the score with common sense to understand its strengths and limitations (such as confidence limits, effect of other factors, etc). What recommendations do you have for doctors once they have applied the UKELD Score? Therefore, it may be used inappropriately as it is an aid, not an absolute prediction. The model applies to death from liver failure and does not apply to many cases, such as cancer, hepatopulmonary syndrome, etc. The score uses lab measurements which are not standardized the components do vary and can be affected by non-liver factors.
What pearls, pitfalls and/or tips do you have for users of the UKELD Score? Do you know of cases when it has been applied, interpreted, or used inappropriately? The MELD Score, a well-respected model, was developed for patients in the US and predicting survival in a slightly different cohort. Why did you develop the UKELD Score? Was there a particular clinical experience or patient encounter that inspired you to create this tool for clinicians?We wanted to create a reliable score based on robust data to predict survival of patients listed for liver transplantation in the UK.


 0 kommentar(er)
0 kommentar(er)
